Not all cholesterol tests you get at the doctor’s office are made equal. Find out which ones are better at predicting cardiovascular risk and which ones you should be asking your doctor about.
Cholesterol gets a bad rap. As a molecule it is important in cellular structure and hormone production. In fact, it’s so important that every cell in our body is capable of making cholesterol. Without it we would die.
Because cholesterol is a lipid, and thus hydrophobic, it doesn’t like water. This means it must be carried around in the blood inside particles called lipoproteins (pictured above). This allows cholesterol (the yellow circles in the picture) to be brought to organs such as the brain where it is used to build cell membranes and insulate nerve fibers.
As I described in a previous article, it’s not the cholesterol but rather the lipoproteins that carry them that can become a health problem. Lipoproteins can enter the walls of blood vessels and initiate atherosclerosis, or plaque formation, predisposing people to heart attacks and strokes.
Meet the lipoproteins

Not all lipoproteins have the same atherosclerotic potential. Some are more notorious than others at causing plaque formation. Low density lipoprotein (LDL) is considered one of the most atherogenic particles, followed by VLDL and IDL. It is often called “the bad cholesterol” even though it’s not the cholesterol itself but the lipoprotein particle that gets into trouble.
Even more atherogenic than LDL is a lipoprotein called Lp(a) (pronounced “L – P – little a”). More to come about this extremely atherogenic particle later and why it’s crucial everyone should get tested for it once in their life.
High density lipoprotein (HDL) is a much more complicated lipoprotein. In general, it protects against atherosclerosis. We know that individuals with high levels of HDL particles in their blood are usually healthier than those with low levels of HDL. Because of this it is often referred to as “the good cholesterol” even though, again, it’s not the cholesterol but the lipoprotein particle we should be referring to.
LDLc
When you get a lipid panel at the doctor’s office it’ll tell you your total cholesterol, LDL cholesterol (LDLc), and HDL cholesterol. LDLc is simply the amount of cholesterol packed into these lipoproteins. The number is either measured directly (if non-fasting) or estimated using a calculation (if fasting).
This LDLc test does not tell you the actual number of LDL particles circulating around in the blood. All it’s telling us is how much cholesterol are in these LDL particles. You might be asking, “why do we care about the cholesterol content when logic tells us atherosclerosis should depend on the number of LDL particles in circulation and not about how much cholesterol they’re carrying?” Turns out the concentration of cholesterol is roughly proportional to the number of circulating particles (but not always, as we’ll see). And many years ago this was the best cholesterol test doctors had available.
This is no longer true.
LDLp
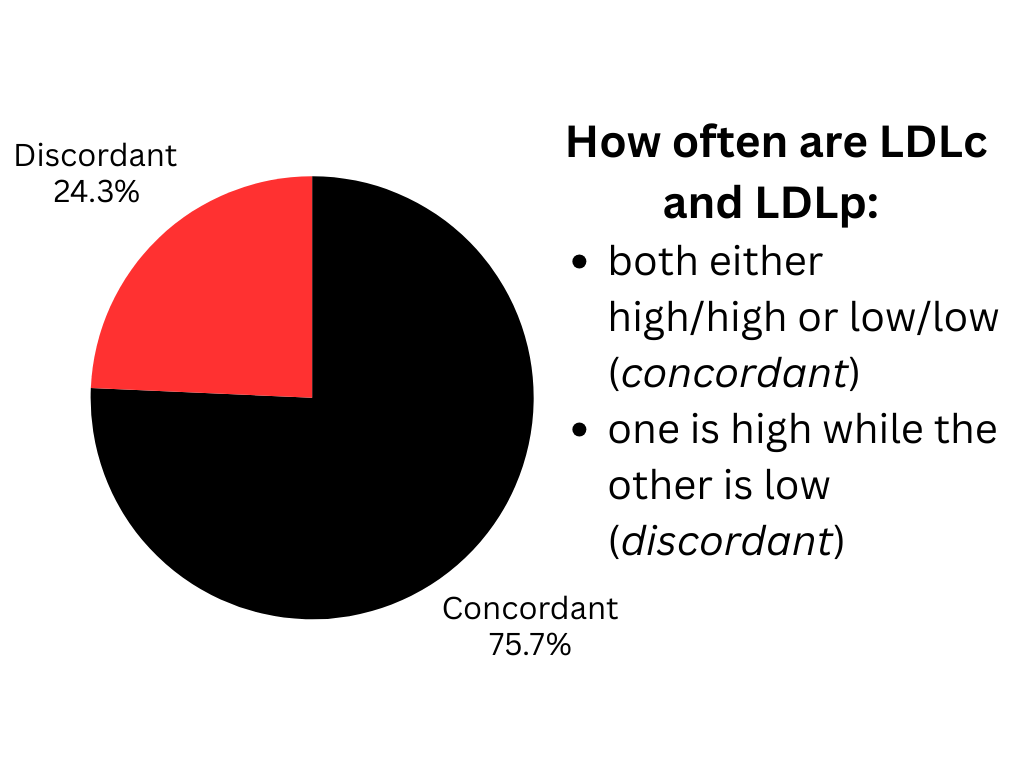
Today, doctors are able to order a cholesterol test that actually measures the number of LDL particles (LDLp) floating around in a person’s blood. Now with two different cholesterol tests available, researchers asked the question how often are LDLc and LDLp in agreement with each other? Studies have shown that they are in agreement about 75% of the time.1 That means that 25% of the time one is high while the other is low!
If LDLp is the superior cholesterol test then that means a quarter of the time doctor’s are getting fooled by a patient’s cholesterol. In the next section on ApoB I’ll explain why LDLp is better than LDLc at predicting someone’s risk of cardiovascular disease.
Mora, Samia, et al. “Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events.” Circulation, vol. 129, no. 5, 4 Feb. 2014, pp. 553–561, https://doi.org/10.1161/circulationaha.113.005873.
ApoB
Apolipoprotein B (ApoB) is a protein present on the surface of the atherogenic lipoproteins: Lp(a), VLDL, IDL, and LDL. (It is the blue blob in the picture at the beginning of this article). There is only one ApoB protein per lipoprotein particle. This means that measuring ApoB tells us the number of, not just LDL particles, but all atherogenic particles floating around in the blood.
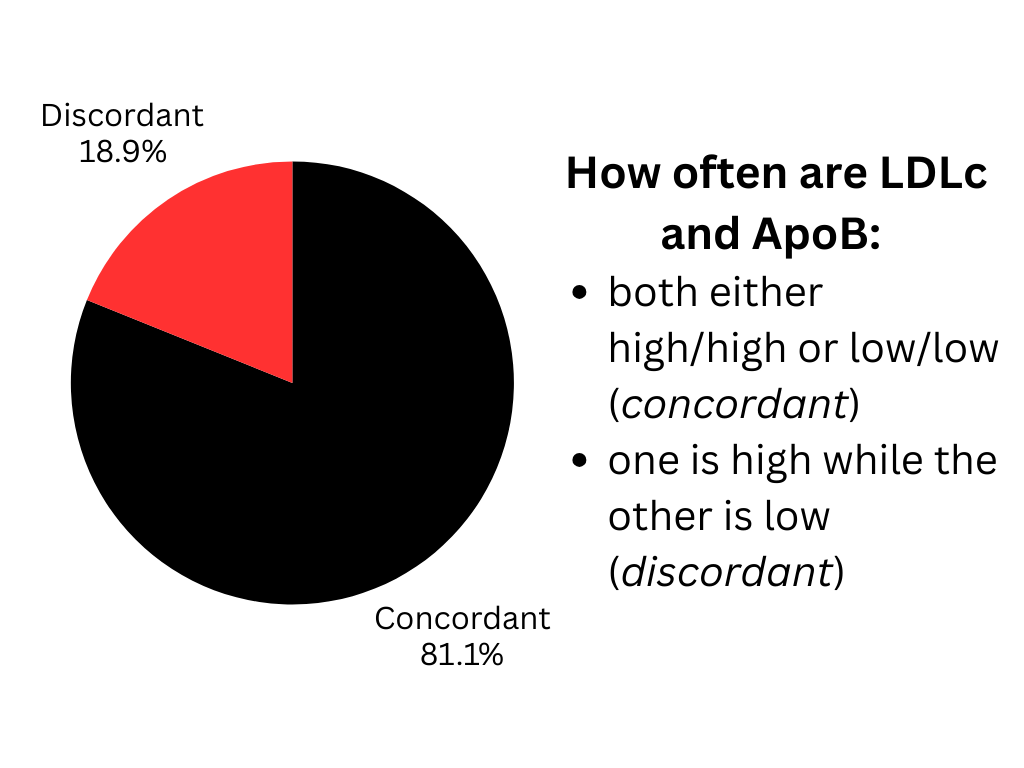
Researchers asked how often ApoB is in agreement with LDLc? They found ApoB to be in agreement with LDLc 81% of the time.2 That means 18% of the time one is high while the other is low. In other words, doctors are being fooled by the LDLc in about a fifth of patients.
But which test is actually better? Ie. which test is better at predicting someone’s risk of cardiovascular disease? Researchers followed the “discordant” population over time (the 18% of individuals with high ApoB and low LDLc or vice versa). They found that ApoB was significantly better at predicting the development of cardiovascular disease such as heart attack and stroke.3 Additional studies have reinforced this finding. For example, a meta-analyses published in Circulation also found that ApoB was superior to LDLc in predicting cardiovascular risk.4
Mora, Samia, et al. “Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events.” Circulation, vol. 129, no. 5, 4 Feb. 2014, pp. 553–561, https://doi.org/10.1161/circulationaha.113.005873.
Lp(a)
Lp(a) is just another lipoprotein like LDL however it is extremely more atherogenic. One study estimated the ability of Lp(a) to generate atherosclerotic plaques to be 6 times more potent than an LDL particle!5 Now that we have been able to identify this troublesome particle, we’ve recognized it to be responsible for a significant number of premature deaths from cardiovascular disease.
Unfortunately, Lp(a) levels in your blood are mostly genetically determined and can’t be lowered even with a stellar healthy lifestyle. Even more troublesome, at the time of writing this article we do not have effective drugs at lowering Lp(a) (however there are drugs being developed in the pipeline).
Even without having much therapies to offer those with elevated Lp(a), simply knowing one’s Lp(a) score can change how we approach other modifiable cardiovascular risk variables. I would personally favor aggressively controlling ApoB, blood pressure, systemic inflammation, and metabolic health compared to others with normal Lp(a) levels.
Key Takeaways
- Because atherosclerotic risk is more influenced by the number of atherogenic particles in the blood rather than the concentration of cholesterol in the particles, ApoB and LDLp cholesterol tests are better than LDLc.
- By using LDLc as a cholesterol test, doctor’s are misclassifying patient’s risk of cardiovascular disease up to 25% of the time.
- Everyone should get their Lp(a) checked once in their life.
References
- Mora, Samia, et al. “Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events.” Circulation, vol. 129, no. 5, 4 Feb. 2014, pp. 553–561, https://doi.org/10.1161/circulationaha.113.005873. ↩︎
- Mora, Samia, et al. “Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events.” Circulation, vol. 129, no. 5, 4 Feb. 2014, pp. 553–561, https://doi.org/10.1161/circulationaha.113.005873. ↩︎
- Mora, Samia, et al. “Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events.” Circulation, vol. 129, no. 5, 4 Feb. 2014, pp. 553–561, https://doi.org/10.1161/circulationaha.113.005873. ↩︎
- Sniderman, Allan D., et al. “A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk.” Circulation: Cardiovascular Quality and Outcomes, vol. 4, no. 3, May 2011, pp. 337–345, https://doi.org/10.1161/circoutcomes.110.959247. ↩︎
- Björnson E, Adiels M, Taskinen MR, Burgess S, Chapman MJ, Packard CJ, Borén J. Lipoprotein(a) Is Markedly More Atherogenic Than LDL: An Apolipoprotein B-Based Genetic Analysis. J Am Coll Cardiol. 2024 Jan 23;83(3):385-395. doi: 10.1016/j.jacc.2023.10.039. PMID: 38233012; PMCID: PMC7616706. ↩︎
