The leading cause of morbidity and mortality is preventable. Learn what you can do to take heart disease off the table.

Without even knowing you, if I had to guess one thing that is most likely to be the cause of your death it would be heart disease. Heart disease is the leading cause of death in the United States and globally. If it doesn’t outright kill you, it will likely cripple your healthspan by decreasing functional ability and causing pain and discomfort.
Although some may consider heart disease a problem of old age, it is actually a slow process that begins at birth. It is true that when looking at age groups heart disease doesn’t become the leading cause of death until you’re over 65 (cancer barely beats out heart disease in ages 45 – 64). However, the disease process actually starts during childhood. In the PDAY study published in JAMA in 1999, they found that by age 20 about 20% of young people had fatty streaks in their coronary arteries. They also found that by age 30, about 10% of individuals had advanced atherosclerotic lesions.
What causes heart disease
Although not the focus of this article, a quick background on how heart disease happens will make the following prevention strategies make more sense. From the moment we’re born we have circulating particles called lipoproteins that carry around cholesterol in the blood. The first step in the process is when the inner layer of cells within the blood vessels get damaged. This damage can come from high blood pressure and things that cause inflammation like smoking.
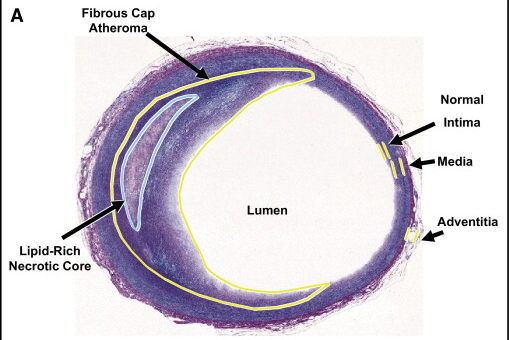
Now, the circulating lipoprotein particles are able to penetrate the damaged blood vessel wall. In general, the higher the concentration of lipoprotein particles in the circulation, the more likely they are to wander into the blood vessel wall and stay there. This kicks off a chain reaction of processes that eventually leads to the formation of plaques in the blood vessel wall. This is known as atherosclerosis. If the plaques get big enough, they can break apart and cause clots to form. If the clot happens in the heart it’s a heart attack. In the brain it’s a stroke.
This entire process is very slow, taking decades to go from the initial step of blood vessel damage to finally culminating in a heart attack. However, give the blood vessels enough damage, enough cholesterol-carrying lipoproteins, and enough time, and this disease process is guaranteed to manifest to some degree in everyone. To decrease the risk of developing heart disease, we need to reduce damage to our blood vessels which most commonly comes from high blood pressure and inflammation and reduce the amount of cholesterol-carrying lipoproteins in circulation.
Controlling blood pressure
High blood pressure increases the risk of atherosclerosis because high pressures inside blood vessels cause damage to the inner wall. Years and years of high pressures inside these delicate blood vessels lead to tiny tears in the walls. Cholesterol can then move through these tears and get stuck inside causing plaque formation.
There are a number of factors that contribute to an individual’s blood pressure (BP). Factors that we can’t control include:
- Genetics – high blood pressure runs in families
- Age – BP tends to increase with age
- Other medical problems – issues like kidney disease can raise BP
However, the list of modifiable factors we can control is longer:
- Diet – low salt diet can lower BP by 6 / 3 mmHg 1
- Aerobic exercise – regular cardiovascular exercise like running can lower BP by 7 / 5 mmHg 2
- Weight – if you’re overweight, losing 5% of your weight can decrease BP by 5 mmHg 3
- Alcohol – one drink daily can increase BP by 2 mmHg 4
- Smoking – quitting smoking can lower BP 4 / 2 mmHg 5
- Chronic stress – prolonged stressors can increase BP up to 10 mmHg 6
- Sleep – poor quality sleep and sleep apnea can increase BP up to 10 / 5 mmHg 7
No excuse for high blood pressure in 2025
The ideal blood pressure for minimizing atherosclerotic risk is a number less than or equal to 120/80. Class 1 hypertension (high blood pressure) is 130-139/80-89. In general, for blood pressure readings consistently in the Class 1 range we would want to consider blood pressure lowering drugs if lifestyle factors have proven unsuccessful. The good news is there are plenty of safe and effective blood pressure lowering medications that can keep you in the optimal range. Unfortunately, only half of adults living with high blood pressure are currently taking medication according to the CDC.8 This means that roughly 60 million people are living with a blood pressure that is slowly damaging their blood vessels and contributing to atherosclerosis. With all the tools we have available to keep blood pressure in the optimal range for longevity, there is no excuse for this number to not be zero.
Controlling inflammation
Inflammation increases the risk of developing atherosclerosis similarly to high blood pressure in that inflammation damages the inner walls of blood vessels. In addition vessel wall damage, it increases the inflammatory reactions that lead to plaque accumulation. Keeping systemic inflammation to a minimum is optimal in preventing atherosclerosis. The list of causes of systemic inflammation is endless. Common modifiable etiologies include smoking, dietary intolerances, autoimmune diseases, and chronic infections.
Smoking
Inhaling smoke directly irritates the lungs leading to an inflammatory response with the release of inflammatory mediators. Cigarette smoke also contains free radicals that damage cells through oxidative stress and indirectly promote inflammation. Its without surprise that smokers have elevated inflammatory biomarkers such as CRP and IL-6 in their blood.9
Dietary intolerances
For some people, the microbiome and/or immune cells that live in their gut don’t always agree with everything they eat. The food sensitivities that cause inflammation in the gut can contribute to systemic inflammation in the body. Common culprits include gluten found in grains and lactose found in dairy. Other are sensitive to foods in the FODMAPS diet which stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. For some, eliminating certain foods in the FODMAPs diet can decrease gut inflammation and thus systemic inflammation.
Autoimmune disease and chronic infection
Those individuals living with autoimmune disease such as lupus or rheumatoid arthritis are predisposed to higher levels of inflammation. It is important to control these diseases by regularly following with a physician who manages them, such as a rheumatologist. Additionally, chronic infections that may go undetected and thus untreated like HIV, hepatitis, STDs, and others contribute to systemic inflammation. You may consider discussing with your physician if you’re at risk for some of these diseases and whether to test for them.
Controlling cholesterol
When the inner walls of the blood vessel become damaged from high blood pressure or inflammation, cholesterol-carrying particles called lipoproteins are able to float into blood vessel wall. Often, they don’t end up leaving. And worse, they kick off a series of reactions that lead to formation of plaque in the vessel wall. To minimize the risk of this happening, ideally we would keep the number of lipoproteins in circulation to a minimum. Less lipoproteins in our blood means there’s a smaller chance of one of them wandering into a blood vessel wall.
High cholesterol factors that we can’t control include:
- Genetics – high cholesterol runs in families
High cholesterol factors that we can control include:
- Saturated fat – decreasing saturated fat consumption can lower cholesterol up to 12% 10
- Exercise – regular aerobic exercise can lower cholesterol 5-10% 11
- Weight loss – if you’re overweight, losing 10% of body weight can correspond to a 10% decrease in cholesterol 12
No excuse for high cholesterol in 2025
Personalization of cholesterol goals based on an individual’s unique attributes is important, but in general, the lower the cholesterol the better. I will go into laboratory tests to monitor cholesterol levels in another article. However, whether you’re following LDLc, LDLp, or ApoB, the lower the value means the lower the risk of developing atherosclerosis. In addition, it would be prudent for everyone to have their Lp(a) tested once to help gauge their risk of atherosclerosis. For most people, lifestyle modifications will not be enough to lower cholesterol levels enough to not have to worry about developing atherosclerosis. The good news is there is a vast number of safe and effective cholesterol lowering medications available today. The small risk of side effects (which often go away when you switch to a different medication) must be weighed against the guarantee of developing atherosclerosis when living with high cholesterol.
The information provided in this article is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
References
- https://www.cochrane.org/CD004022/HTN_effect-low-salt-diet-blood-pressure-and-some-hormones-and-lipids-people-normal-and-elevated-blood ↩︎
- https://www.health.harvard.edu/diseases-and-conditions/how-does-exercise-affect-blood-pressure ↩︎
- https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/managing-weight-to-control-high-blood-pressure ↩︎
- https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/expert-answers/blood-pressure/faq-20058254 ↩︎
- https://www.tobaccoinduceddiseases.org/The-role-of-smoking-cessation-programs-in-lowering-blood-npressure-A-retrospective,142664,0,2.html#:~:text=Results%3A,12.0%20mmHg%2C%20from%20the%20baseline. ↩︎
- https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/stress-and-high-blood-pressure/art-20044190#:~:text=There’s%20no%20proof%20that%20stress,too%20much%20alcohol%20or%20caffeine. ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3666153/ ↩︎
- https://www.cdc.gov/nchs/products/databriefs/db511.htm ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1160597/#:~:text=Smoking%20triggers%20an%20immunologic%20response,markers%20predict%20future%20cardiovascular%20events. ↩︎
- https://pubmed.ncbi.nlm.nih.gov/9101427/#:~:text=Diets%20provided%2034%25%20fat%2C%2015,increase%20in%20LDL%2Dreceptor%20number. ↩︎
- https://www.healthline.com/health/high-cholesterol/treating-with-statins/best-exercises ↩︎
- https://www.webmd.com/cholesterol-management/cholesterol-and-weight ↩︎
